Your body has 24 spinal discs. They are located between individual vertebrae in your back and neck, and have tough exteriors with soft, gel-like interiors creating cushions between the bones in your back.
Your spinal discs function as shock absorbers for your body keeping your vertebrae separate when your body jars from impact and activities.
When you experience problems with one or more of your discs, it can have quite a few negative impacts on your life with the following types of symptoms:
- Difficulty sleeping
- Diminished quality of life
- Impaired mobility
- Inability to work
- Muscle weakness
- Pain
The precise symptoms you experience vary according to the specific types of disc problems you’re living with. Some spinal disc problems are caused by injuries, while others develop as a result of aging.
This guide will help you better understand the types of spinal disc problems — and their respective treatment, so you can make informed decisions about your condition.
Call today
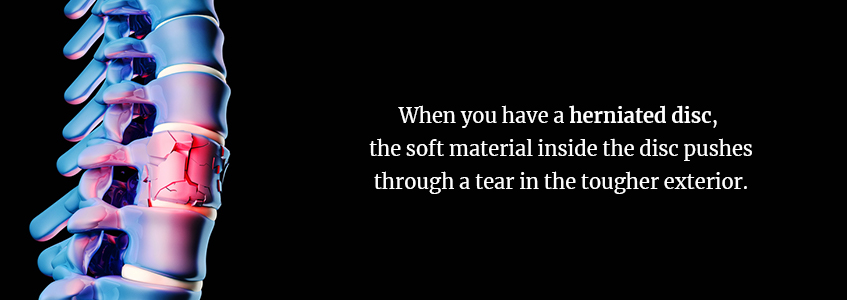
1. Herniated Disc or Slipped Disc
One of the more common disc problems is known as a herniated disc, sometimes also referred to as a slipped disc or ruptured disc. When you have a herniated disc, the soft material inside the disc pushes through a tear in the tougher exterior. It sometimes irritates nearby nerves, causing you to experience pain and a variety of other symptoms.
Symptoms of a herniated disc vary from one person to the next. You may experience many or none of the symptoms listed below if you have a herniated disc:
- Arm pain
- Leg pain
- Numbness
- Tingling
- Weakness
While often the result of aging, herniated spinal disc problems may also be the result of improperly lifting heavy objects. If you lift with your back instead of your legs or twist or turn while lifting heavy objects, you could end up with a herniated disc.
Occasionally, herniated discs may result from traumatic events, like falling or blows to the back.
You are at greater risk of developing a herniated disc if you are overweight, work in a physically demanding job, or have a family history of herniated discs.
You have a variety of treatment options available for your herniated disc included several non-surgical treatments, such as:
- Acupuncture
- Hot and cold therapy
- Massage therapy
- Over-the-counter medications
- Physical therapy
- Prescription medications, including narcotics, anticonvulsants and muscle relaxers
- Steroid injections
- Yoga, for gentle stretching and strengthening the core
In rare cases, surgery, which may be minimally or least invasive, may be required to deliver relief from your herniated disc and its associated pain.
2. Pinched Nerve
While a pinched nerve can occur throughout your body, having a herniated disc is one of the most common causes of a pinched nerve. For instance, if you have a herniated disc in your lower spine, it may place pressure on the nerve root, which causes radiating pain shooting down the back of your leg.
Symptoms of a pinched nerve include:
- Feeling as though affected limbs — legs, feet or hands — have fallen asleep
- Muscle weakness
- Numbness in areas affected by the nerve
- Pins and needles sensations in affected areas
- Sharp, aching or burning pain radiating outward
Pinched nerves occur when excessive pressure is placed on your nerves by surrounding tissues. This can be caused by a variety of things, including:
- Bone spurs
- Certain illnesses, such as diabetes, thyroid disease or rheumatoid arthritis
- Herniated disc problem
- Hobbies
- Injuries
- Obesity
- Repetitive motion from work
Your physician may recommend physical therapy as well as anti-inflammatory medications to manage the pain from your pinched nerve. They may also suggest corticosteroid injections to manage the pain and inflammation. In some cases, surgery or a minimally invasive procedure by one of our experts to remove or shave a bone spur or treat a herniated disc may be required to address the root cause of the pinched nerve.
3. Bulging Disc
While some people mistake herniated discs from bulging discs, they’re different back disc problems. With a herniated disc, the tough membrane surrounding your disc is ruptured, allowing the soft substance to leak through.
If you have a bulging disc, you have a bulge along the circumference of one of your discs but the tough membrane hasn’t ruptured. These bulges often appear along the rear and side portions of your discs, placing pressure on the nerve and creating pain.
Bulging disc symptoms may include:
- Burning
- Difficulty walking
- Heaviness
- Numbness
- Pain
- Tingling
- Weakness
Depending on the location of your bulging disc, you may experience these symptoms in different regions of your body. For instance, if your bulging disc is in the lumbar region, you may experience these sensations in your lower back, legs, buttocks and feet. If it is in your cervical region, you may experience these symptoms in your neck, arms or hands. In some cases, you may even encounter them in your head.
With thoracic spine bulging discs, which are far less common, you may experience upper back pain radiating throughout your stomach or chest. This type of pain is often mistaken for cardiovascular problems. Do not dismiss this lightly if you do experience chest pain as a result of your back disc problems.
Age, neck strain, back strain, injuries from accidents or falls and genetic factors can cause bulging discs. Conventional treatments for bulging discs include:
- A period of not lifting heavy objects or engaging in demanding physical activities
- Chiropractic care
- Hot and cold therapies
- Lifestyle changes
- Over-the-counter or prescription medications
- Rest
- Spinal decompression therapy
- Steroid injections
- Stretching exercises
- Weight loss
Sometimes, surgery or a minimally invasive procedure in our office by one of our experts is necessary to offer definitive relief from the pain and pressure of a bulging disc, though open spine surgery is only recommended as a last resort once you’ve exhausted all other treatment options.
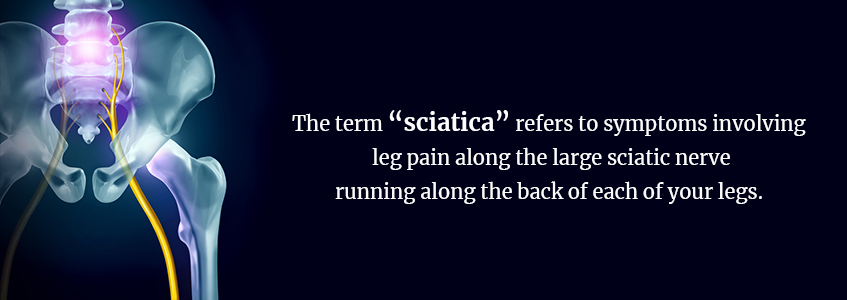
4. Sciatica
The term “sciatica” refers to symptoms involving leg pain along the large sciatic nerve running along the back of each of your legs. This pain often accompanies tingling, numbness and weakness originating in your lower back and traveling all along the back of your leg.
Sciatica is not a medical condition itself, but instead, is the symptoms of another medical condition. Contributing medical conditions may include:
- Degenerative disc disease
- Herniated discs in your lumbar region
- Spinal stenosis
- Spondylolisthesis
Symptoms of sciatica are fairly consistent. You may experience one or more of the following if you’re living with the pain of sciatica:
- Constant pain on one side of your leg and buttock — note that this condition rarely affects both legs
- Leg pain that is often more pronounced when sitting
- Leg pain you might describe as burning, searing or tingling
- Radiating pain traveling down the back of one leg and possibly into your foot and toes
- Sharp pain making walking and standing painful
The pain from sciatica may be infrequent and irritating or it can become constant and incapacitating depending on the location of the affected nerve. You may have a greater risk of developing sciatica if you are older, overweight, have diabetes, work in a physically demanding job or work in a job requiring long periods of sitting.
Treatments for sciatica often involve treating the underlying condition and may include:
- Acupuncture
- Chiropractic manipulations
- Epidural steroid injections
- Exercise
- Hot and cold therapies
- Massage therapy
- Over-the-counter medications
- Physical therapy
- Prescription medications
Sometimes, it’s necessary to treat the underlying condition with surgery though sciatic itself rarely requires surgery, as it is a symptom of another ailment rather than a medical condition in itself.
5. Spinal Stenosis
Spinal stenosis is a narrowing of the open spaces of your spine. It is most commonly located in the lower back and the neck. When this occurs, it places pressure on nerves traveling through the spine causing a variety of unpleasant symptoms which may worsen over time.
Symptoms of spinal stenosis vary according to the location of the narrowing. If you have cervical spinal stenosis occurring in the neck, you may experience:
- Difficult walking
- Loss of bowel or bladder control in severe cases
- No sense of balance
- Numbness and tingling of your hands, arms, feet or legs
- Pain in your neck
- Weakness in one of your hands, arms, feet or legs
Lower back spinal stenosis symptoms vary somewhat and may include the following:
- Back pain
- Numbness or tingling in one of your feet or legs
- Pain or cramping in one or both legs upon standing or walking for long periods, usually easing upon bending forward or sitting
- Weakness in one or both of your feet or legs
Because many potential causes for spinal stenosis exist, you should consult your physician if you suspect you have this condition to rule out other culprits, which include herniated discs, overgrowth of bone, thickened ligaments, tumors and spinal injuries.
People over the age of 50 are at greater risk of spinal stenosis though you may be affected at a younger age as a result of congenital spinal deformities, genetic diseases affecting bone and muscle development or trauma.
Treatments vary widely according to many contributing factors. You will work with your doctor to determine your best choice from options such as:
- Hot and cold compresses
- Physical Therapy
- Over-the-counter and prescription medications
- Steroid injections
- Minimally invasive lumbar decompression procedures (Vertiflex and/or Endoscopic Laminotomy)
In some cases, surgery is a necessary solution to treat your spinal stenosis and provide relief from the pain it causes.
6. Degenerative Disc Disease
As you age, the discs in your spine begin to show signs of wear. While not everyone does, you may develop degenerative disc disease as a normal part of your aging process. While not necessarily a disease, it is a condition caused when the damage to your discs causes you pain. This happens because your discs have low blood supplies and are unable to repair themselves once injured.
If you have degenerative disc disease, your symptoms may include some or all of the following:
- Numbness and tingling in your extremities
- Pain worsening while sitting, bending, lifting or twisting
- Relief from pain when walking or running, changing positions frequently or lying down
- Weakness in your leg muscles
- Periods of severe pain — lasting days or even months — before recovering and later returning
- Pain ranges in severity from nagging to completely debilitating
The natural aging process is the primary cause of degenerative disc disease since your discs naturally deteriorate as you age. Certain activities and factors can place additional stress on the spinal column and may accelerate the damage to the discs. These include:
- Frequent lifting
- Obesity
- Poor posture
- Repetitive Bending
- Sports accidents
- Traumatic injuries
- Twisting
You have treatment options available to you for the pain associated with degenerative disc disease. They include:
- Epidural steroid injections
- Hot and cold therapies
- Manual manipulation or chiropractic care
- Massage therapy
- Over-the-counter medications
- Physical therapy
In some cases, you may have extensive pain or damage that cannot be corrected with non-surgical remedies. In these instances, surgery or a minimally invasive endoscopic procedure by one of our experts may be your only viable option for lasting relief from the pain of degenerative disc disease.
Treatments for Spinal Disc Problems at the Spine INA
Treatment options for spinal disc problems have advanced, offering new relief for old pains. This means you have more options than ever before to treat your spinal disc problems. Consider learning about the least-invasive treatment options available at the Spine Institute of America. These include:
1. Endoscopic Spine Surgery
Endoscopic surgery is often appealing because it is a minimally invasive procedure allowing you to receive relief from the pain of a herniated disc by removing the damaged disk and cleaning up the surrounding area endoscopically. Outpatient endoscopic spine surgery requires no sutures, only a small bandage over the incision.
2. Regenerative Medicine
On their own, your discs are unable to regenerate themselves efficiently. The new frontier of regenerative medicine, though, involves helping them to regenerate through a variety of methods. Regenerative medicine procedures we offer include:
- Platelet-Rich Plasma Injections (PRP): PRP injections activate your body’s stem cells. Your own blood is spun down and added to a highly-concentrated mixture of growth factors designed to stimulate your stem cell activities. The mixture is injected into the site of your injury to help repair the damaged discs.
- Prolotherapy: This type of treatment involves injecting natural irritant agents into the area to initiate a regenerative response in the surrounding tissues. While they would not regenerate on their own, the irritant incites the regeneration process in your discs, promoting healing.
3. Minimally Invasive Lumbar Decompression (MILD)
This procedure involves a very small incision to treat the narrowing of the spinal canal as seen in spinal stenosis. MILD avoids the use of invasive fusion surgery and helps to eliminate the risk of spine instability. It enables you to have a quick recovery and fast pain relief.
4. Neuromodulation Therapy
Here, neuromodulation therapy involves overpowering your pain signal to provide relief. Procedures we offer in neuromodulation therapy include:
- Transcutaneous electrical nerve stimulation (TENS): TENS offers short-term pain relief by passing alternating electrical current through superficial tissues.
- Peripheral nerve stimulation: This therapy helps to control pain by using electrodes on your peripheral nerves.
- Spinal cord stimulation: Designed to mask pain signals before you can feel them, physicians may use this therapy for failed surgeries, chronic pain and more.
- Dorsal root ganglion (DRG) stimulation: This procedure stimulates nerves to help block pain signals.
5. Vertiflex
This procedure is a small implant between the spinous processes to relieve the symptoms of spinal stenosis.
Of course, there are more invasive surgical procedures available as well. You must work closely with your doctor to determine the best treatment for your condition and your quality of life.
What Should You Do When Traditional Spinal Disc Treatments Fail?
For many people, traditional treatments for disc problems may offer reprieve given enough time and proper rest. However, if you have tried the traditional treatments and aren’t finding the relief you seek or are wanting the least invasive treatment options for spinal disc problems instead of open back surgery, then look to us here at the Spine INA.
We specialize and are leaders in providing revolutionary, least invasive treatments for your back pain and disc problems. We offer endoscopic procedures, regenerative medicine, neuromodulation therapy and more, so you have options not involving risky spine surgeries, fusions and long recovery times.
Call the Spine INA in New Jersey today at (609) 371-9100 to learn more about your least invasive treatment options for disc pain relief or book your appointment through our online form.
Schedule a consult








Leave a Reply